Are you a Healthcare Professional?
The information contained in this section of the website is intended for US healthcare professionals only. Click CONFIRM to confirm that you are a healthcare professional.
"(Required)" indicates required fields
You are about to leave the ISTURISA.com website and enter a website operated by an independent third party. The links to third-party websites contained on ISTURISA.com are provided solely for your convenience. Recordati Rare Diseases does not control the opinions, claims or comments contained on any third-party website linked to ISTURISA.com, and your activities at those websites will be governed by the policies and practices of those third parties.
Cushing’s disease is a rare disease that can pose many challenges—from getting diagnosed, to handling the physical and emotional toll it can take, to finding the right treatment. But this is a journey you don’t have to take alone.
No matter where you are in your journey, you likely have questions. Cushing’s disease is not a straight pathway. There are likely twists and turns along the way. In addition to reaching out to your doctor, you can find answers to your questions right here.
Your doctor has likely diagnosed you with Cushing’s disease after finding a benign (noncancerous) tumor on your pituitary gland (found at the base of your brain). As you may know, one of the jobs of the pituitary gland is to tell other glands what to do, and that includes telling the adrenal glands to make cortisol. Cortisol is a hormone that helps control your mood, motivation, and the way you feel when you’re scared of something. That’s why it’s often referred to as the “stress hormone.”
While we all need cortisol to live, this tumor causes the adrenal glands to make too much cortisol, which leads to the symptoms of Cushing’s disease. The goal of any treatment for Cushing’s disease is to get your cortisol back to normal levels.
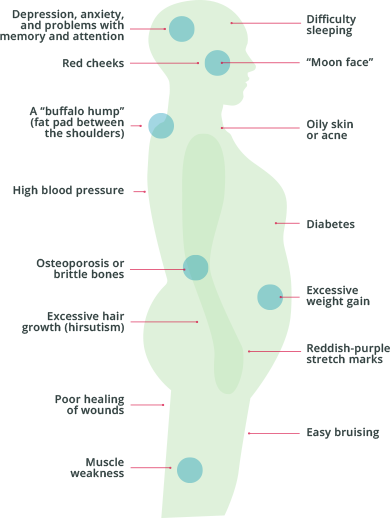
By now, you know the symptoms you have been feeling are a result of Cushing’s disease. While your symptoms may be different from someone else’s, there are some symptoms that typically occur. You may have experienced some or all of these common symptoms at one time or another. If your Cushing’s disease has gone away and come back, you may even have different symptoms now than in the past.
The goal of any treatment for Cushing’s disease is to bring your cortisol levels back to normal. Surgery to remove the tumor on your pituitary gland is often the first choice of treatment. If surgery isn't successful, then a combination of surgery and multiple medicines may be used.
The surgery for Cushing’s disease is called transsphenoidal surgery, or TSS. It’s a very specialized surgery, so it’s important to find a neurosurgeon who has done many of these before.
It’s important to know that even if the surgery works well, you may not feel better right away. That’s because it takes time for cortisol levels to return to normal. Your doctor may recommend cortisol replacement therapy until this happens.
Unfortunately, surgery doesn’t always work for everyone. And, even years after surgery, Cushing’s disease can come back. That can be very disappointing. But there are other things you can do—including taking ISTURISA, a medicine specifically made to treat Cushing’s disease—that can help you take control of your disease.
Having surgery offers hope of a more normal life. The reality is that surgery does not work for everyone. And even if it does work for some time, Cushing’s disease can come back. That can be very disappointing and affect your mood and quality of life.
But there are other things that you can do to take control of your Cushing’s disease, by lowering cortisol levels in your body. Medicines are available that target different areas: the tumor on the pituitary gland, the adrenal glands, or the cortisol receptors throughout the body. Medicine may be one option that may be needed in your treatment journey.
In addition to medicines and a potential second surgery, other treatment options that you may have tried or that your doctor may recommend include
Radiation therapy—Radiation to the pituitary tumor may help control the tumor growth and lower cortisol levels. You should know that it can take years for radiation to work. During this time, your doctor may suggest medicines to help bring down your cortisol levels.

Removal of the adrenal glands—Surgery can be done to remove the adrenal glands. But this is only recommended if other treatments don’t work or if you are very sick. That’s because once your adrenal glands are removed, your body doesn’t make any cortisol at all. You will need to take multiple medicines to replace this.
Wherever you are in your journey with Cushing’s disease, if you are unsure of anything or want to learn more about treatment options, like ISTURISA, which was made specifically to treat Cushing’s disease, be sure to talk with your healthcare provider. There are ways for you to treat your Cushing’s disease.
 ISTURISA is a medicine that is specifically made to treat Cushing’s disease by lowering cortisol levels
Learn more
ISTURISA is a medicine that is specifically made to treat Cushing’s disease by lowering cortisol levels
Learn more
ISTURISA (osilodrostat) is used to treat adults with Cushing’s disease who cannot have pituitary surgery, or who have had pituitary surgery, but the surgery did not cure their Cushing’s disease.
To report SUSPECTED SIDE EFFECTS, contact Recordati Rare Diseases Inc. at 1-888-575-8344, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Before taking ISTURISA, tell your doctor about all of your medical conditions, including if you:
Tell your healthcare provider about all the medicines you take, including prescription medicines, over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take medicines used to treat certain heart problems. Ask your healthcare provider if you are not sure whether your medicine is used to treat heart problems.
Please see the Full Prescribing Information, including the Medication Guide, for ISTURISA and talk with your healthcare provider.
The information contained in this section of the website is intended for US healthcare professionals only. Click CONFIRM to confirm that you are a healthcare professional.
You are now leaving the ISTURISA® (osilodrostat) website. This link will take you to a site maintained by a third party who is solely responsible for its content.